Featured Post
Who Can Own a Medical Spa?

Show your committment to patient safety, legal compliance and community over competition.
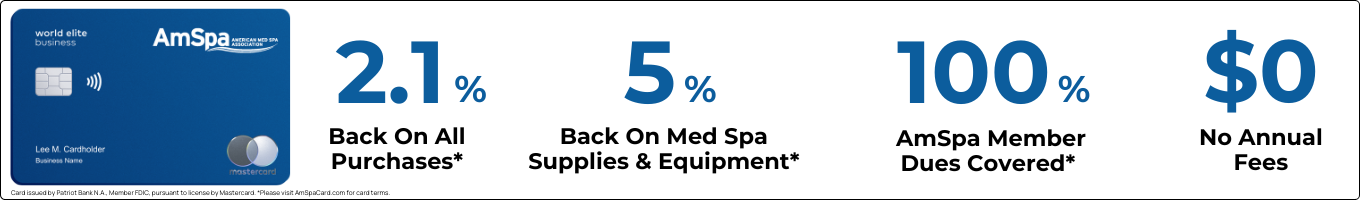
AmSpa members receive preferred pricing on all AmSpa live and virtual trainings.
Get the latest news and information about safe, legal practice in medical aesthetics directly in your inbox.
Get access to med spa laws, in-person and online training and more!

Clinical
Win Free Exosomes → Simply Register for the Free Exosome Masterclass By MedResultsIn today’s rapidly evolving aesthetic landscape, one ...

Legal
If you’re running a medical spa, you probably wear a dozen hats before lunch, provider, HR, marketing, IT, therapist, and ...

Marketing
By Growth99The med spa industry is experiencing a profound transformation, and it's creating two distinct categories of practices: those strategically ...

Software
By Eric Atienza, Assistant Director of Digital Marketing and Marketing TechnologyRunning a small medical spa often means doing everything yourself ...

Marketing
By AestheticsPro For medical spa owners looking to reach their clients in the most...
Top Tags
January 24, 2023
Figure displays medical aesthetics industry annual revenue ($ in billions). By Madilyn Moeller Day-to-day life...

February 24, 2021
By Bradford E. Adatto, Partner, ByrdAdattoIntravenous (IV) therapy has been used to provide nutrition and...

September 21, 2023
By Patrick O'Brien, JD, General Counsel, American Med Spa Association [AmSpa first published a...

July 19, 2023
By Patrick O'Brien, General Counsel, American Med Spa Association (AmSpa) UPDATE #2 (2/08/2024): Since...